
Finley was born via C-section due to a few complications. I was almost 42 weeks pregnant, and my body was not ready to give birth yet. Her heart rate started to drop when we were hooked up to the monitors, and that’s when the doctors decided it was time for the C-section. Finley came into the world as a “normal” baby. While we were still in the hospital, my husband and I had some concerns about her eyes and how rigid she seemed, but we were reassured that these were just “normal baby movements.” I was a first-time mom and had nothing to compare it to, so we trusted the doctors. Still, something in my gut felt off.
We were discharged from the hospital, and we thought we were on our way home to start our new life together. That night, while I was breastfeeding, Finley vomited bright green. Before we left the hospital, they had warned us to go to the ER immediately if her vomit was bright green or red. So, we rushed her to the ER, and she was admitted. They ran a series of GI tests, but everything came back normal. We were monitored for a while but were eventually sent home.
The next day, we had her first pediatric appointment, where she received her first vaccination. About 45 minutes to an hour after the appointment, my husband noticed something was wrong. He was holding her, and she seemed spaced out and rigid. Her little hand was clenched so tightly that we couldn’t pry it open. I was exhausted, still healing from my C-section, and brushed it off, thinking it was probably nothing. I told him, “If it happens again, we’ll take her back to the hospital.”
Around 3 or 4 a.m. that morning, I happened to wake up and looked over at her. She was having another episode. Panic set in, and we gathered everything and rushed back to the ER. That ER visit was a nightmare; there’s no other way to put it. They ran every test imaginable—spinal taps, EKGs, EEGs, MRIs, blood samples, and urine samples. I’m sure there were others, but they did everything they could. Finley had more episodes during our time there, and they quickly admitted us.
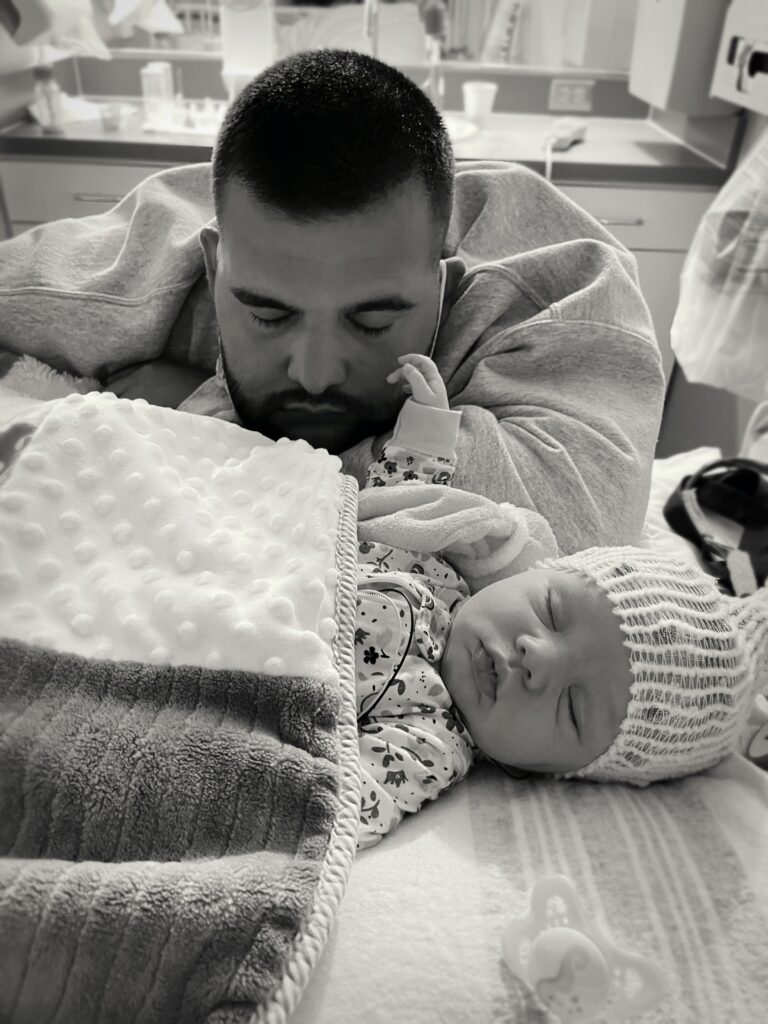
While waiting for the neurology team to arrive, Finley went into crisis. Her oxygen levels were dropping, and her heart rate spiked to over 200. The doctors administered the standard medication for newborn seizures, which stopped her body from convulsing, but her brain continued to seize. They told us to call our support system because things were not looking good. They planned to intubate her so they could administer stronger drugs, but they needed her tiny body to be still. At that moment, I think we realized just how serious this was. My husband and I clung to each other, preparing ourselves for the unimaginable—life without Finley.

Walking into the PICU and seeing my newborn baby hooked up to machines, with tubes down her throat, was like an out-of-body experience. I was still healing myself, but all that mattered was getting our sweet girl healthy again. Thankfully, we had an incredible doctor, Dr. Brown, who just happened to be on call that week. He was the calm in our storm. They called him in the early hours of the morning to check on Finley, and he administered a range of medications, including B6. Little did we know, that was exactly what her body desperately needed.
We spent 3 to 4 days in the PICU. Once they got a clean EEG for the desired duration, they slowly began removing the tubes and equipment. Each removal was a victory, a step closer to going home as a family. Dr. Brown had also ordered a genetic panel while she was hospitalized, but we had to wait 6 to 7 weeks for the results. During that time, we kept a whiteboard, meticulously writing down every medication dose and noting how she was doing. Looking back, I’m sure she was heavily sedated on all those drugs, but we were doing everything we could to keep her safe.
The day we got the results, our medical team called immediately. They connected us with specialists, and we learned that Finley had pyridoxine-dependent epilepsy (PDE). We started her on triple therapy shortly after, and since then, she has been thriving. She hasn’t had a seizure since those early days, and for that, I thank God and the incredible doctors who saved her.
Every day is still a challenge. Being a mom is hard enough, but when you’re constantly worrying about what they eat, when they need their medication, what developmental milestones they might be behind on, and how they will handle each day, it’s incredibly draining. For a long time, we felt alone in this journey. We didn’t know any other PDE families until we were introduced to Curtis and the PDE Foundation. Kristy and her son Jaxson were the first people we connected with, and I will be forever grateful for her coming into our lives. Our first conversation was a long, emotional phone call that lasted hours, and I’ll never forget it.



Finding this community has been a game-changer for our family. The sense of belonging and being able to talk to other families who understand our daily struggles has been incredibly emotional, but in the best way possible. We now have an incredible support system, an army of people fighting for our kids, and I’m so grateful to be a part of it.
 Donate
Donate